A recent Duke study lends insight into why some individuals with autism have reduced pain sensitivity.
Using a mouse model of autism developed in the lab of Yong-Hui Jiang, associate professor of pediatrics and neurobiology, the study linked a mutation in the gene SHANK3 to the reduction of the pain receptor TRPV1. The study—which also involved the lab of Ru-Rong Ji, professor of anesthesiology and neurobiology—will help researchers and physicians develop more effective interventions for those with autism.
“We know that human patients with SHANK3 deficiency have autism,” Jiang said. “It’s very common for patients with autism in general to have a kind of reduced pain sensitivity or sensory processing problems.”
Ji explained that altered pain sensitivity in individuals with autism had already been well-established before the latest experiment. However, the mechanism behind the decreased sensitivity remained a mystery until now.
Earlier in 2016, Jiang’s lab developed a mouse model of autism that accurately replicated the mutation of the SHANK3 gene. These SHANK3-deficient mice were the subjects of this most recent experiment investigating pain sensitivity.
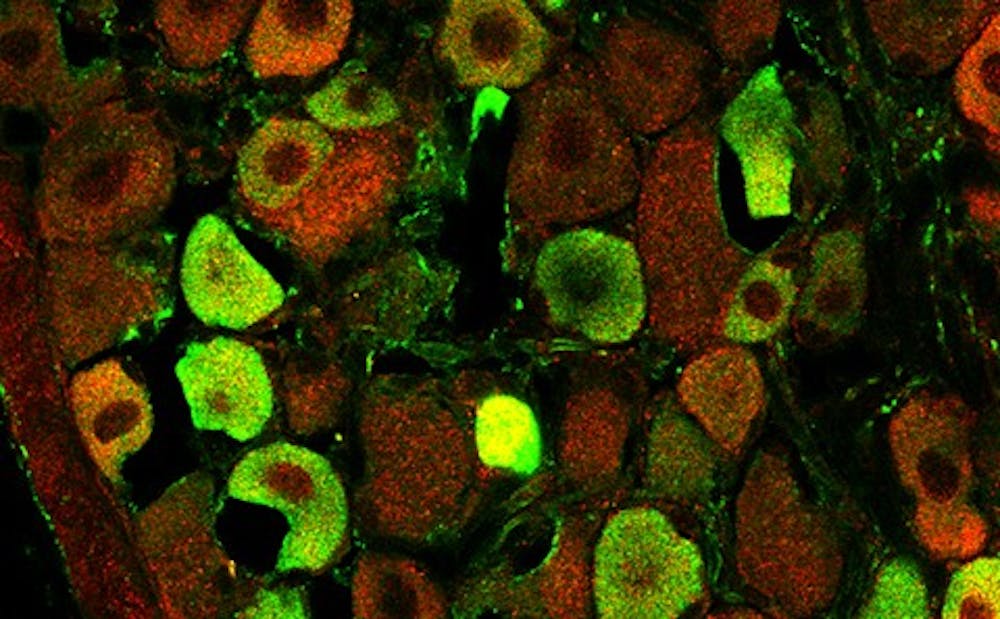
The researchers put the mice through different sensory tests and found that they had lower sensitivity to heat-related pain. They discovered that missing SHANK3 lowered TRPV1’s ability to transmit pain signals. TRPV1 is a receptor protein capable of detecting and transmitting pain signals caused by capsaicin, the chemical that gives peppers their spiciness.
“If you lose SHANK3, TRPV1 cannot function properly,” Ji said.
In addition to the link between SHANK3 and TRPV1, the study also revealed that TRPV1 is present in the presynaptic terminal—the neuron that sends a pain signal—in addition to the postsynaptic terminal—the neuron that receives the signal.
However, Jiang noted that researchers are still unsure of the significance of TRPV1’s presence at the presynaptic terminal.
Another interesting observation was the expression of the SHANK3 gene in a cluster of neurons in the peripheral nervous system known as dorsal ganglia neurons. Previously, only the role of SHANK3 in relation to the central nervous system—the brain and spinal cord—had been studied.
“Most people investigating the field believe that most [autistic] behavior is CNS-related, not PNS-related,” Jiang said.
Geraldine Dawson, director of the Duke Center for Autism and Brain Development, noted that the many treatments currently being investigated at Duke are focused on the CNS.
“These treatments are different approaches to improving brain function,” Dawson wrote in an email. “For example, one study is exploring whether umbilical cord blood can improve outcomes for young children with autism.”
Ji and Jiang both said they are hopeful that the discovery of the SHANK3/TRPV1 relationship may ultimately benefit both autistic and non-autistic individuals.
“We can develop new therapeutics to target the interaction between these two proteins for non-autistic patients with chronic pain,” Ji said.
Jiang noted that a different treatment could target autistic individuals with a SHANK3 mutation—approximately one percent of those with autism—and stabilize their ability to feel pain.
“What we hope is that by studying a rare form of autism, we can inform a more generalized knowledge about other types of autism,” Jiang said. “Eventually, we can develop a more universal understanding of how autism develops and how to develop a more universal intervention.”
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.