A new program is providing students who have eating disorders with specialized treatment avenues aimed to minimize disruption of their lives.
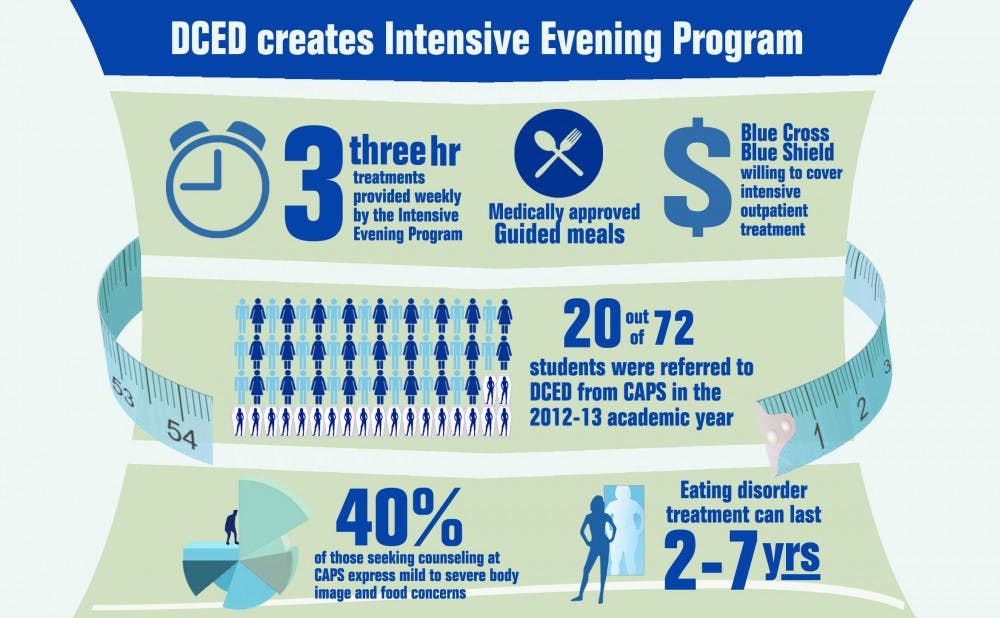
The Intensive Evening Program at the Duke Center for Eating Disorders provides comprehensive care to students who have moderate to severe symptoms of disordered eating without forcing students to take a medical leave. Opened to Duke students two weeks ago, the program provides patients with treatments over the course of three three-hour weekly sessions—all covered by the University’s insurance policy. Counseling and Psychological Services will assess and refer students who have severe symptoms of disordered eating to the program.
“Eating disorders are severe mental illnesses that can be life-threatening,” said Nancy Zucker, director of the Duke Center for Eating Disorders. “The impetus for this program was to see if it’s possible to provide more intensive care while keeping students matriculated at Duke.”
In the 2012-13 academic year, CAPS provided assessments for 72 students, and referred 20 to the DCED for specialized care, said Paula Scatoloni, the eating disorder coordinator at CAPS.
“It’s been pretty good,” said Danna Alvarado, a nursing student suffering from anorexia nervosa who was referred to Zucker’s care five months ago by CAPS. “The people not only at CAPS but also Dr. Zucker’s program really care.”
The Intensive Evening Program provides nearly 10 hours of care each week to patients during which their medical status is monitored by physicians from DCED. Each treatment day of the week, patients participate in guided meals, where a group of physicians provide support while the patient is given a medically-approved meal.
When symptoms of disordered eating become severe, patients often become medically unstable and require hospitalization. Inpatient care provides intense therapies to patients in an isolated environment, Zucker explained. Individuals coming out of inpatient settings often find they are unprepared to handle real-world scenarios, which leads to relapse.
“The difference between being in an inpatient setting and being in the real world is vastly different, and relapse rates for people coming out of inpatient treatment in the first year is very high,” Zucker said. “We’re actually giving folks tools that they can then practice that day, the next day… and then have a buffer of support in the evening.”
During the 2012-13 academic year, nearly 40 percent of the students who sought treatment at CAPS had mild to severe body image and food concerns, Scatoloni said.
“CAPS is actually not an appropriate place to treat eating disorders because we only offer short-term support,” Scatoloni said. “We’re actually doing [students with intense eating disorder symptoms] a disservice by treating them at a college counseling center for something that needs a specialized service center.”
She added that treatment for patients with severe eating disorder symptoms is often complex and can last between one and seven years—a type of treatment that the Eating and Body Image Concern team within CAPS was not created to do and does not have the resources to carry out.
Blue Cross Blue Shield—the insurance provider for students—has supported efforts to develop an intensive outpatient therapy for students, said Sue Wasiolek, dean of students and assistant vice president for student affairs.
“[Representatives from BCBS] were readily willing to cover the intensive outpatient treatment that is offered through Dr. Zucker’s office,” Wasiolek said, adding that research on the therapy has been promising.
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.