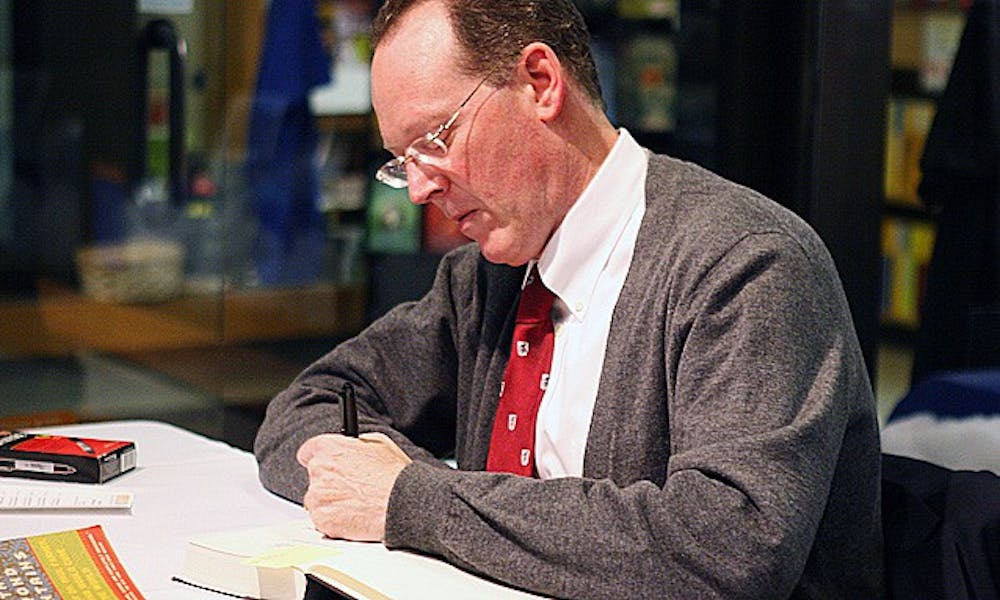
Medical anthropologist, physician and the author of numerous books on health and human rights Paul Farmer spoke at Duke Saturday about his book “Haiti After the Earthquake.” Farmer is the Kolokotrones University Professor and chair of the department of Global Health and Social Medicine at Harvard Medical School, member of the Duke Board of Trustees and the Duke Global Health Institute Board of Advisors, a Trinity ’82 graduate and former writer for The Chronicle. He is also the founding director of the Boston-based organization Partners in Health—expanding access to health care in 12 developing nations. The Chronicle’s Ashley Mooney and Julian Spector sat down with Farmer to discuss his experiences in global health.
The Chronicle: Can you tell us about the state of global health when you got into the game?
Paul Farmer:. The roots of what your generation calls global health are in international health, and the roots of that are in colonial and neocolonial health. There were very tight ties between health, trans-regional commerce and military ventures. Global health is really much more about health disparities and health equity. Sometimes those disparities happen locally, like the difference between a wealthy part of Durham and a poor part of North Carolina. Duke Engage, by the way, is really about disparities. [Duke students] live in a forest; it’s like a “Gothic Wonderland.” If you don’t engage beyond the boundaries of the campus, that’s not a good thing.
TC: How do you think the Partners in Health approach has contributed to this overall shift over the past couple of decades?
PF: It’s a small organization compared to a lot of other players—we only help in 12 countries—but we have a fairly large impact because we keep focusing on equity. If someone says, “You can’t treat AIDS in Africa; they’re too poor,” we’re going to be the first to say that’s not true. Poverty doesn’t need to be the chief determinant of whether or not someone gets health care. You have to put in systems that are not just the commodification of medicine. If we just accept that you buy health care as just a commodity—if it’s a public health problem and you’ve privatized it—that’s a problem.
TC:What role did poverty play in the earthquake in Haiti?
PF: Poverty was a big part of the earthquake because there were no building codes, so the houses were very shabbily constructed. Even before the earthquake, people were at risk because they lived in substandard buildings that couldn’t take the shock. All along the way were many opportunities to intervene so that social disparities don’t affect the body. Haiti also needed better immediate access to rescue and relief after a natural disaster.
TC: What was so fascinating to you about Haiti, even when you were an undergraduate?
PF: I was already writing about Haitians when I was at Duke—I wrote an article called “Haitians without a Home.” I had received an award to go to Haiti when I graduated in 1982, and it changed my life completely. I was part of a grassroots organization that later became Partners in Health. The clinic I worked in was very substandard—people would line up to see only one doctor. I saw that people were not getting the medicines they were prescribed because they couldn’t pay for them, so I did a study of 100 patients. It was something like only 20 percent of them actually had their prescriptions filled correctly. Why? Because they didn’t have money at the pharmacy. So that’s the idea that we later adopted at PIH—we don’t sell drugs, they’re part of the care package.
TC: When you’re working in a world with scarce resources, how do you ultimately deal with the model of just giving people drugs?
PF: Have we ever worked in a time where there aren’t scarce resources? Have we lived in a time when there are abundant resources for the people most at risk of being sick? Not that I know of. We always live on a planet where there are scarce resources. The average cost in the United States to treat AIDS is approximately $10,000 per patient per year. In Africa, we’re paying $100 per patient per year. It’s not like God hands down the price of a vaccine on a stone tablet. We set the prices based on things like production capacity, demand and economies of scale, so basically all of [this] can cost whatever we want. It’s all things that are subject to human control. The people who are selling AIDS drugs for $100 a year are still very profitable. The guy’s a multimillionaire who did it.
TC: How do you stay motivated in the face of seemingly endless challenges in your line of work?
PF: I teach and I meet young people. The metaphor the Haitians use is “behind mountains there are more mountains,” which means there’s always more work to be done. The only way to get more work done is to bring more people in to do the work, right? Twenty-six years ago, not many people were interested in global health, but now there are plenty. So that’s how you keep going.
TC: What do you see as the current biggest challenges in global health?
PF: One of the biggest problems is financing, because the failure of imagination has been accentuated by a global economic downturn. Global health has been starved of resources forever, it’s never had the proper level. The biggest challenge is resource constraint, but that’s not as big as it was before. Resource constraint means human resources, too—nobody was interested in poor people’s health, and there was a lack of imagination and lack of tools that we needed. A lot of those problems have not been solved, but they’re much better. So failure of imagination is number one, and... is tied to us being socialized for scarcity. The socialization for scarcity is [when] we assume that lower standards for poor people are acceptable.
TC: How do you convince people to fund drugs that, for example, cost $10,000 in the United States but $100 in a different country?
PF: One thing that I think is best to do in my line of work is to assume that people do care about other people. More than half of all American households contributed to earthquake relief in Haiti. Some say that the most noble sentiment that we have as a species is solidarity—you care about someone even if you don’t know him or her. And there’s an even better kind of solidarity—pragmatic solidarity. I believe that most people want to see the fruits of science and technology shared with others. If you assume that people don’t care, then this work is doomed.
TC: Is there almost more willingness to tackle these problems in developing countries than at home?
PF: Health care in the United States is messed up. We spend more than any other country, and we don’t get good results—we rank nowhere near the top in many categories. There is more social space in which to move freely in [developing] countries, and there are fewer institutions that are obstructionist. So, yes, there is more willingness [there], but we have more resources, and we have a lot of talent in health care.
TC: Many donors made a pledge to Haiti that hasn’t been fulfilled yet. How do you see that going?
PF: People are forgetting already about the earthquake. I think funding from them is definitely still a possibility, and we need to make it happen. We need to support those in Haiti, and make sure we don’t let up. That’s also why I’m here—to remind people about how much there is to do.
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.