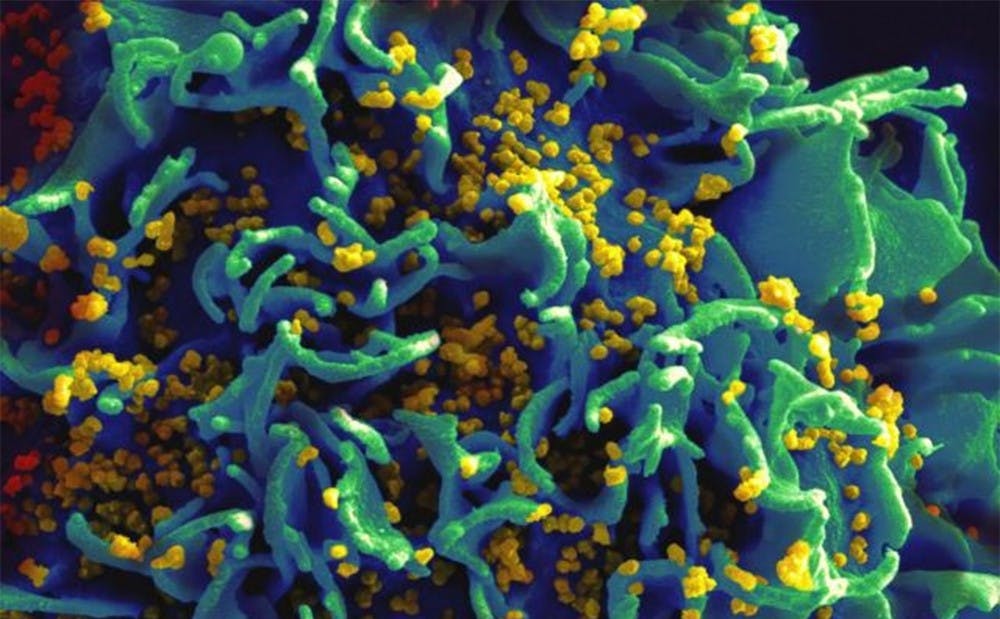
A discovery made by Duke researchers is shedding light on a potential new strategy for producing an effective HIV vaccine.
The human body is capable under certain conditions of creating broadly neutralizing HIV-1 antibodies, or bNAbs, to fight the virus. Led by Dr. Barton Haynes, director of the Duke Human Vaccine Institute, a team of researchers have studied 100 people infected with HIV—half of whom naturally produced bNAbs and another half that did not. This was done with the goal of inducing bNAbs in people without HIV as a potential vaccine, Haynes said.
“We’re talking about developing a preventative HIV vaccine whereby we give the vaccine to someone who has not become infected, so that they will not become infected,” he said.
This new work builds off prior discoveries by Haynes and his team. In March, Haynes co-authored a study identifying an HIV patient with "broadly neutralizing antibodies," which imitated T-helper cells and prevented the virus from spreading.
Haynes explained that bNAbs resemble the antibodies found in patients suffering from autoimmune diseases. In those patients, "the body lacks control over making antibodies that cross-react with their own cells," he said.
Because of this potential cross-reaction, the body has evolved to be wary of such antibodies, Haynes explained, which makes inducing their creation more difficult.
“That’s a trait of bNAbs, they don’t hurt the person but it’s a sneaky strategy,” he said. “Not all antibodies that cross-react with human tissue are dangerous. But the body doesn’t know that and doesn’t want to try to do that.”
This high risk explains why bNAbs capable of fending off a HIV infection have typically only been found in the immune systems of people who already have the virus, when it might be too late.
By the time a HIV infected body feels besieged enough to risk producing bNAbs, the virus has already progressed to the stage where it is latent and hiding in the cells, explained Dr. Tony Moody, chief medical officer of the DHVI. The latent virus essentially becomes invisible to the immune system. This can happen even days after an infection, he said.
"Once that latent pool is established, the immune system has a hard time eliminating it because the latent pool causes the virus to hide," Moody noted. "So even if your immune system does a great job in eliminating all the cells it can see, there are still cells hanging on that as soon as pressure is taken off, the cells can start churning out virus again and continue the infection.”
In short, by the time the body overcomes its evolutionary wariness towards bNAbs and decides to deploy these antibodies as a last resort, it might be too late for the bNAbs to do any good.
But discovering why the body does not deploy bNAbs until too late gives researchers a better chance of determining how they may induce their production in those not yet infected, Haynes noted.
“Knowing this is what’s going on this is good for us, this is very helpful," Haynes said. "Because now we can figure out how to guide the immune system to go around this roadblock.”
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.