Overall patient volume and revenue at Duke University Health System have fallen in the past fiscal year, reflecting the current economic climate and national changes to health care.
The decrease in patients has occurred in several major areas, including emergency room visits, surgical cases and endoscopy cases. DUHS leaders attribute the decline to increased competition in the region, driven by the economy and the Affordable Care Act. Health professionals in private practice are looking to align themselves with bigger health systems with more financial security, taking their patients with them. Additionally, the slow economy has driven more people to avoid medical visits because of the cost.
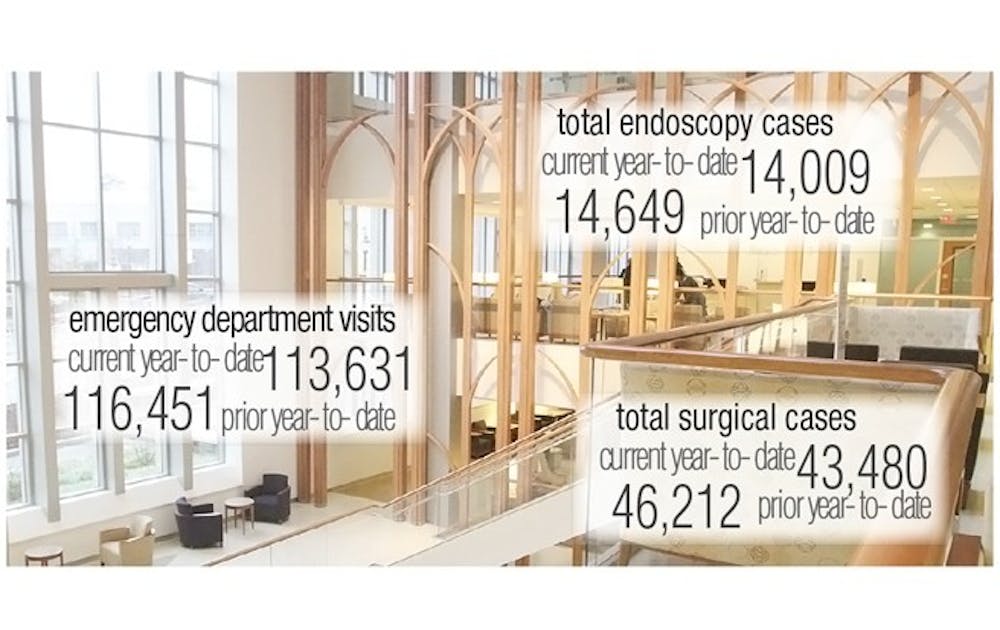
The decrease in patient volume resulted in a drop in revenue. Compared to the same point in the previous fiscal year, total surgical cases have decreased by 2,732, total endoscopy cases decreased by 640 and emergency department visits have decreased by 2,820, according to data from Kenneth Morris, senior vice president, chief financial officer and treasurer of DUHS. DUHS expected to bring in $1.467 billion in revenue in fiscal year 2013 by the end of January, but fell $31 million short at $1.436 billion.
The reduction is indicative of a trend that has hurt hospitals nationwide, said Dr. Victor Dzau, chancellor for health affairs and president and CEO of DUHS.
“It’s a country-wide phenomenon,” Dzau said. “We seem to be better insulated here—the effects are not that bad... For Duke, overall, we are doing very well.”
The effects of assimilation
The Affordable Care Act, in combination with the current economic climate, has placed “enormous pressure” on private health care providers to align themselves with bigger health systems like DUHS to gain competitive advantage in attracting patients, Morris said.
Whereas there used to be a “free market” for specialty referrals, in which patients often visited different providers for various treatments, patients now stay primarily within the larger health system with which their providers have aligned themselves. As a result, DUHS has seen a decline in patients who follow their doctors elsewhere.
“People tend to stay within their own systems,” said Dr. Robert Califf, vice chancellor for clinical and translational research and director of the Duke Translational Medicine Institute. “If you have a lot of private care practices that are now owned by Duke or [the University of North Carolina at Chapel Hill], those practices tend to refer in their own system.”
As competing institutions lure physicians to practice at their facility as opposed to a competitor’s, DUHS must constantly compete to gain and retain physicians and keep their patients along with them.
“Community doctors come and go based on where they can have the best meal for themselves,” Executive Vice President of DUHS Dr. William Fulkerson said. “They are being asked to choose sides—where do they want to align to ensure their practices are competitive?”
Additionally, a high unemployment rate has also decreased patient volume as people forego getting elective medical procedures that they cannot afford.
“North Carolina is running over a 9 percent unemployment rate, and majority of those folks don’t have health insurance, so they will likely delay elective procedures or discretionary procedures until they are employed and have insurance,” Fulkerson said. “That’s something we’ve seen across the country.”
Challenge areas
This competitive nature has hurt Duke Regional Hospital more than other hospitals within DUHS, pushing Duke Regional to “build back up,” Fulkerson said. He did not comment on the exact decrease in patients. Kerry Watson, president of Duke Regional Hospital, could not be reached in time for publication.
Additionally, the Duke Cancer Center, which has been open for a little more than a year, did not reach its target patient volume, Dzau said, though he did not specify by how much. Despite falling short of this goal, the center has grown by 1-2 percent this year, he added.
“The Cancer Center continues to be in a ramp-up phase, responding to the increasing volumes of new cancer cases in our community,” Duke University Hospital President Kevin Sowers wrote in an email Monday.
Inpatient to outpatient
Using more outpatient care than inpatient care has caused a decline in patient volume at Duke and other hospitals, Fulkerson said. For example, several years ago a patient getting his or her gall bladder taken out would be hospitalized for a couple of weeks. Nowadays, patients undergoing that surgery will go home the next day.
As such, inpatient care is decreasing as outpatient care increases.
“It’s less expensive to do outpatient care,” Fulkerson said. “We reserve inpatient care for patients who really have a very significant level of illness now. We can accomplish more on the outpatient side than ever before, but that means inpatients are sicker than 10 to 20 years ago.”
Physicians are also driven to provide better outpatient care because a component of the Affordable Care Act penalizes hospitals that readmit a patient within four weeks for reasons that should have been treated on the previous visit.
The focus on increased outpatient care could explain a decrease of patients visiting the emergency room, Califf added.
“If you provide much better outpatient care you are going to reduce your number of emergency room visits from complications like strokes and other factors,” he said.
‘We will be paid less’
DUHS initiated an effort to reduce costs in 2008 in order to increase financial sustainability. Since its initial launch, however, DUHS leaders have begun looking into other areas to cut costs.
“We have to anticipate that in the future we will paid less for what we do, so there is a tremendous imperative for us to decrease our costs and continue to grow in terms of patient volumes by presenting clinical services that are highly desirable and produce terrific results,” Fulkerson said.
To reduce costs going forward, DUHS leaders have looked at the partners they have bought drugs from and whether better prices can be negotiated, he said, adding that they have also looked at ways to deliver care at lower costs.
Another way to decrease costs is to identify barriers that have hindered patient discharge and resolve them.
“We are going to have to deliver the same kind of quality with less financial support in the future, so getting smarter about what we do and making sure we are not wasting money will be very important,” Fulkerson said.
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.