A collaborative effort to reduce diabetes in the South will receive a major boost from the federal government.
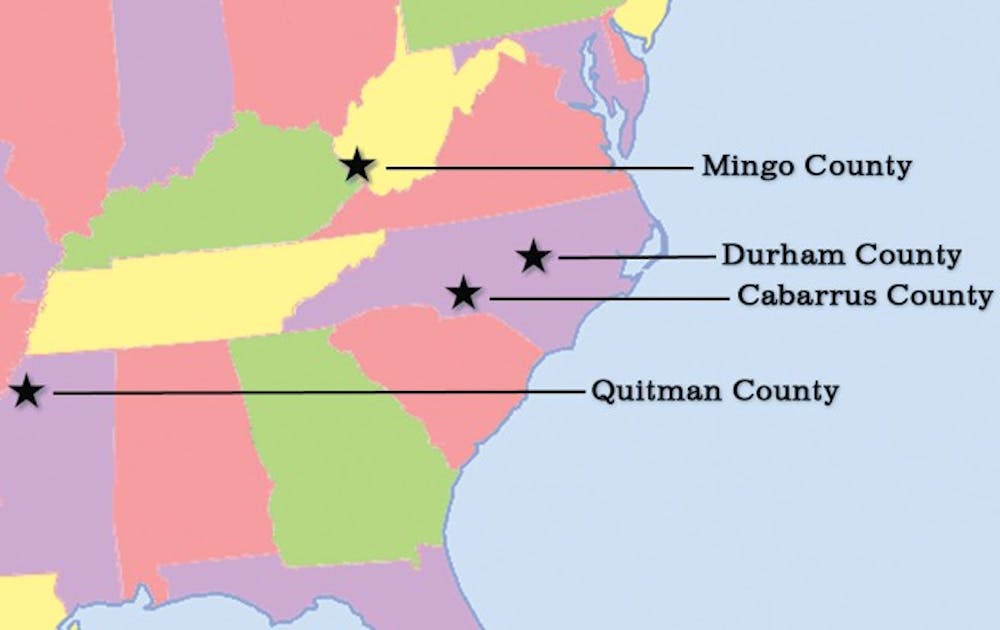
The Duke University Medical Center and the University of Michigan’s National Center for Geospatial Medicine are partners in “From Clinic to Community: Achieving Health Equity in the Southern United States,” an effort to bring more community-based care to counties where Type 2 diabetes is particularly prevalent. The plan, which focuses on patient-centered care, is among the preliminary Health Care Innovation Award recipients. Given by the Center for Medicare & Medicaid Innovation Center, the approximately $9.7 million award will be implemented to spearhead programs in four underserved Southeast counties: Durham County, N.C.; Cabarrus County, N.C.; Quitman County, Miss. and Mingo County, W.Va.
Within these regions, the money will be used toward the delivery of medical care to the homes of people with Type 2 diabetes, said Dr. Robert Califf, vice chancellor for clinical research at Duke and leader of the project.
“Type 2 diabetes is a massive epidemic now that is having a huge toll on death and disability globally, but especially in the Southeast of the United States,” Califf said. “For people within those life circumstances—and there are a lot of them—we have layers of people who can help that are actually in the neighborhood and can stop by your house and check on you.”
Medical care needed to help people with complications from diabetes—such as cardiac procedures and dialysis—is extremely costly, Califf said, adding that a reduction in diabetes in the four counties is estimated to save $20 million alone.
The plan will rely on technology created by Califf and Marie Lynn Miranda, director of Michigan’s National Center for Geospatial Medicine, which has an office in Durham.
The technology makes use of an electronic health record driven by geospatial referencing to determine which members of a particular community need more intensive care, Califf said. Geospatially enabled health information technology is an approach that applies statistical analysis and other informational techniques to geographically based data.
“We start with this sophisticated technology system that combines medical record data and data on the communities where people live to target intervention programs for people living with Type 2 diabetes,” Miranda said. “The data infrastructure helps us understand the different resources available to people in different counties, so we can design different interventions.”
Califf noted that diabetes is a major issue in the Southeast because of the region’s recent urbanization. In a rural county with a large farming community, people are accustomed to a higher calorie intake because of their daily physical exertion. But urbanization promotes a more sedentary lifestyle, which, combined with the same high-caloric eating habits, results in an increased rate of diabetes.
The four counties represent different demographics, Califf added. Durham County and Cabarrus County are both urbanized, whereas Quitman County and Mingo County are rural. Furthermore, the counties represent different racial demographics—with Quitman County largely populated by black people and Mingo County by white people.
“We really will have all the cultural influences in all those four counties culminate. Regardless of which culture you come from, there is this high rate of obesity and diabetes,” Califf said. “That’s the backdrop of why we thought these four areas would be important for a project that is supposed to show how the change in the delivery of health care has a big impact.”
Gayle Harris, director of the Durham County Board Health department, said the award will be used in part to create homecare teams of dietitians, social workers and community health workers. Funding will also be used to set up a diabetes intelligence office that will take the information provided by the geospatially enabled health information technology to raise awareness in certain communities on what people can do to prevent the onset of Type 2 diabetes.
“Winning the award is both a triumph and tremendous challenge,” Miranda said. “The CMS [Innovation Center] has placed public trust in us in the belief that we can make real and meaningful change in our country, and we have to step up to this challenge and make this program work.”
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.