President Barack Obama's calls for national efforts to fight antibiotic resistance are being met by researchers and physicians in Duke hospitals.
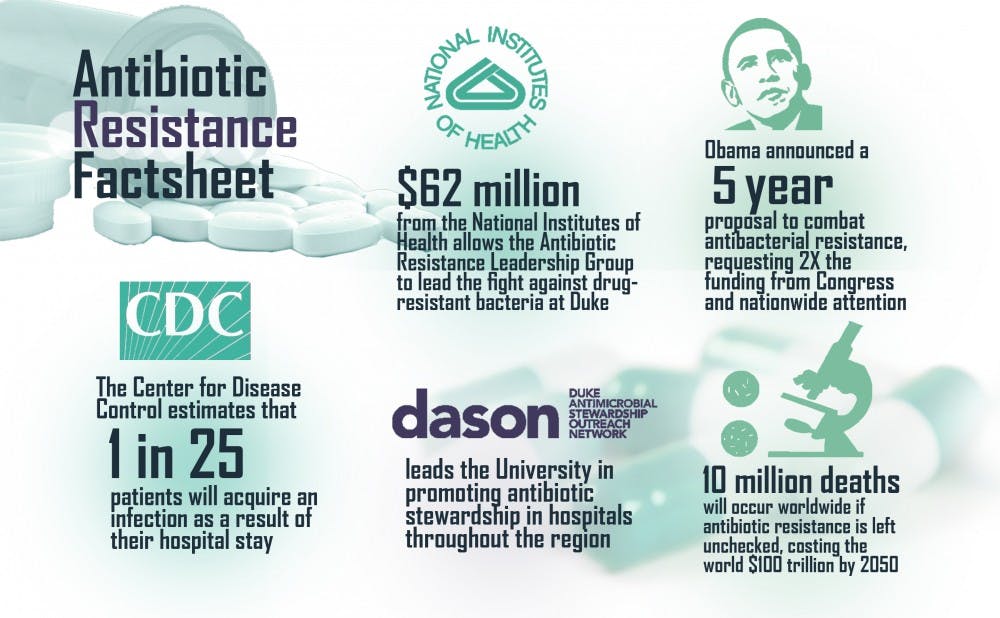
Obama recently announced a five-year proposal to combat the issue of antibacterial resistance, requesting double the funding from Congress amid nationwide attention. The Antibacterial Resistance Leadership Group—funded by a $62 million grant from the National Institutes of Health—leads the fight against drug-resistant bacteria at Duke. Although the issue has been growing over the last several decades, antibiotic resistance's impact on health has now reached a crisis point, said Dr. Vance Fowler, professor of medicine and one of two principal investigators in the ARLG.
“On a general scale, antimicrobial resistance really does pose the specter of a post-antibiotic era, for which there are literally no antibiotic treatments,” Fowler said. “Many doctors have encountered some patients like that already.”
The Centers for Disease Control and Prevention estimates that one in 25 patients will acquire an infection as a result of their hospital stay. Urinary tract infections, skin infections like methicillin-resistant Staphylococcus aureus, respiratory pneumonia and surgical site wound infections are commonly seen today in hospital patients and are becoming harder to treat due to increasing antibiotic resistance.
Hospitals and health systems such as Duke are beginning to implement a number of different strategies to combat this growing problem.
One such strategy is antibiotic stewardship, which relies on doctors to be more judicious in their prescriptions and eliminate unnecessary antibiotic use. The Duke Antimicrobial Stewardship Outreach Network leads the University in promoting antibiotic stewardship in hospitals throughout the region.
“The reality is that treating with antibiotics is an educated guess, at least until you get a culture test back and you identify the bacteria," Fowler said, adding that doctors still never withhold antibiotics from a patient who truly requires them.
Before receiving and interpreting the culture tests, many doctors treat patients with broad-spectrum antibiotics like ampicillin, which can allow resistant bacteria to flourish. Improving diagnostic tests to reduce the amount of time broad-spectrum antibiotics are used on patients is part of the multi-pronged approach employed in the Duke Regional Hospital, explained Dr. John Boreyko, clinical pharmacist at the DRH and co-director of its antibiotic stewardship program.
“We have seen some reductions in resistance,” Boreyko said. “But it takes a whole village.”
Other strategies include promoting hand-washing and hygiene within the hospital and isolating patients who have drug-resistant infections to prevent them from spreading. Part of the difficulty lies in changing the attitude that patients have had for decades, added Boreyko.
“We’re just so ingrained in our belief that if we don’t feel well, we need an antibiotic,” he said. “We have to start asking when we go to see a doctor—do I really need this antibiotic that could cause more harm down the road?”
Even outside of hospitals, communities around the nation are increasingly affected by “explosions” of diseases like MRSA, Fowler noted.
Antibiotic resistance has also proven deadly on a global scale. The rates of infections like multi-drug resistant tuberculosis and malaria are already climbing in countries with less advanced health systems, according to reports by the World Health Organization.
A recent study commissioned by United Kingdom Prime Minister David Cameron predicts that, if left unchecked, antibiotic resistance will be responsible for 10 million deaths worldwide and will cost the world $100 trillion by 2050. The presence of drug-resistant bacteria in human populations, along with a reduction in the number of effective antibiotics and the slow pace of new antibiotic discoveries has led to what Fowler calls “a perfect storm.”
Obama's proposal to combat antibiotic resistance has received nationwide support from doctors and researchers. The proposal features a $1.2 billion investment that will go toward the discovery and evaluation of new antibiotics and diagnostic techniques, increased monitoring of hospital antibiotic use and support for antibiotic stewardship programs.
“This is clearly an issue that’s starting to garner the attention it deserves,” said Dr. Anthony So, public policy professor and director of the Program on Global Health and Technology Access. “But one has to wonder whether the $1.2 billion that’s proposed will be sufficient, if we are to address to full scope of this problem. The national strategy will be a useful starting point though.”
Fowler added that, as a researcher, he is also thrilled that the issue has reached international prominence.
“I’m glad to see that it’s in the limelight, and I’m very glad to be at Duke where we can be a part of the effort to combat it," he said.
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.