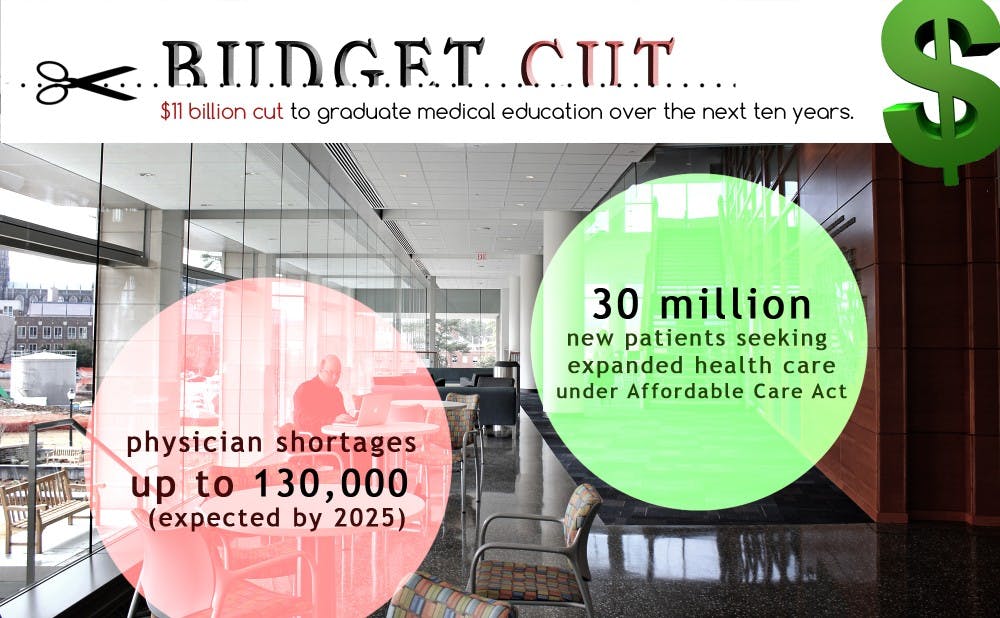
The 2014 budget proposal, which will cut funding to train medical residents over the next 10 years, will not only decrease the capacity of residency programs, but might also limit the ability of teaching hospitals to provide residency care for certain patients, said Victor Dzau, chancellor for health affairs and president and CEO of the Duke University Health System. If passed, $780 million will be cut in the year 2014 alone.
To show their protest to the cuts, several Duke medical students met with Rep. David Price (D-N.C.) to bring the potential impact of the cuts to his attention.
“These cuts could decrease the already limited residency training spots available for U.S. medical graduates and prevent the expansion of the physician workforce to meet the growing patient demand,” said Benjamin Streufert, a third-year medical student and president of the Duke School of Medicine American Medical Association and a member of the North Carolina Medical Association Student Chapter.
Physician shortages of up to 130,000 are expected by 2025, Streufert noted, while 30 million new patients will be seeking expanded access to health care under the Affordable Care Act. Current levels of funding for residency programs, however, are not expected to keep pace with that growth.
Traditionally, residency funds are distributed in many ways. Some money goes directly to paying residents’ salaries, but a good amount goes to supporting the infrastructure—the equipment, teaching physicians and supervising personnel—necessary to maintaining a working residency program, Dzau noted.
Cuts to graduate medical education funding will also hurt teaching hospitals like Duke that train residents, said Samara Jinks, a first-year medical student and co-chair of the AMA for the class of 2017.
“Many elderly, uninsured or HIV patients can get treatment at teaching hospitals because they offer disproportionately large amounts of residency care,” Jinks said.
Dzau said that the cuts could threaten Duke’s core mission of teaching, research and clinical care.
“All the pipeline of the next generation of physicians and physician leaders are through the GME program,” he said. “Medical education is an education, so that has to be brought about in the context of a teaching environment and the technology and infrastructure to support that environment.”
On Sept. 24, 22 students from the School of Medicine, most from the class of 2017, sat down with Price as part of a campaign to protect federal funding for graduate medical education.
Although students had already known about the budget proposal much earlier in the year, they waited until now to take action, Jinks noted.
“The national chapter [of the AMA] wanted to make it a concerted effort, set up to be a flood, not a trickle,” she said.
According to Streufert, Price expressed concern about the cuts and their consequences not only for future residents whose jobs are at stake, but also for the patients that need access to the unique care teaching hospitals provide.
Although he was supportive of the students’ efforts to preserve GME funding, Price is keenly aware of the restrictive fiscal climate facing the nation, Streufert said.
Jinks noted that it was ironic that the cuts were proposed just after an effort to solve the physician shortage encouraged medical schools to open their doors to more students.
“Our class is the largest class ever in the history of Duke Medicine—we have 113 students,” Jinks said. “The Fed pushed schools to increase their class sizes but now they’re shrinking the residency program, essentially telling people to train for no job. That’s where the bottleneck happens.”
Dzau said, however, that the medical school looks at undergraduate, graduate and residency education as a continuum, not as individual blocks.
“We are always looking at our class sizes in relation to the capacity of our residency programs to make sure that the pipeline makes sense and avoids bottlenecks,” he said.
Dzau also noted that he was more concerned for the long-term, macro effects of the cuts, adding that the cuts will bring into question the changing roles and need for physicians versus nurse practitioners and physician assistants as reflected in the needs of society.
“The real issue is how will this affect the country’s ability to be a leader in health care and research,” Dzau said.
Regarding the immediate effect of the cuts, however, Dzau said that not much could be done by the school in the way of changing government policies that recur from time to time.
“Duke will always be committed to excellence in GME funding as we have over the years. We have a GME fund set up and will use that,” he said. “The government cut will surely affect us, but it is something we cannot predict and something that will have an impact on Duke and all teaching hospitals across the nation.”
Get The Chronicle straight to your inbox
Signup for our weekly newsletter. Cancel at any time.